The United States faces an unprecedented demographic shift as the baby boomer generation enters their senior years. According to the US Census Bureau, by 2030, all baby boomers will be older than 65. This will expand the size of the older population so that 20% of the US population will be at retirement age. More importantly, by 2034, adults 65 and older will outnumber the population 18 and younger for the first time in the nation’s history. The significant increase in the elderly population has led to a growing demand for senior care services and an evolution in caregiving models. However, challenges remain, such as acute staffing shortages, quality of care, elder abuse, and the impact of unpaid caregiving. In this blog post, we dive into the various types of caregiving prevalent in the US market, rank the top 5 most popular models, and explore emerging industry trends. Be sure to follow us on LinkedIn. Now, let’s get started.
Types of Caregiving Models in the US
The US senior care market has developed a diverse range of caregiving models to meet the varied needs of seniors, from those requiring minimal assistance to those needing round-the-clock care. In-home care has become increasingly popular, allowing seniors to receive assistance while remaining in the comfort of their own homes. This model includes personal care, companionship, homemaker services, and skilled nursing care. The elder care market in the US was valued at $445.49 billion in 2023 and will reach $615 billion by 2029. In 2023, Home Care represented the largest market share at 32%.

Assisted Living Facilities
Assisted living facilities offer a balance between independence and support, providing 24/7 staff assistance, meal services, social activities, and basic medical care. The National Center for Assisted Living reports that approximately 30,600 assisted living communities have nearly 1.2 million licensed beds in the United States. These communities serve over 818,000 residents, with over 50% aged 85 and older. Services provided include:
- 24-hour supervision and assistance
- Exercise, health and wellness programs
- Housekeeping and maintenance
- Meals and dining services
- Medication management or assistance
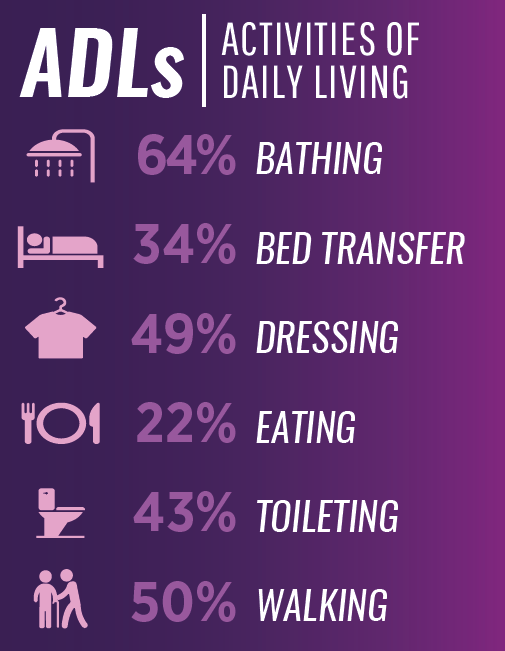
- Personal care services such as Activities of Daily Living (ADLs)
- Arranging for transportation
The majority, 40.8%, of the communities are in the Western US, followed by 28% in the South, 22.6% in the Midwest, and 8.6% in the East.
Nursing Homes
Nursing homes, also known as skilled nursing facilities, provide the highest level of care outside hospitals. According to the Centers for Disease Control and Prevention (CDC), there were 15,600 nursing homes in the US as of 2019, with 1.3 million residents. These facilities offer 24/7 nursing care, rehabilitation, and long-term care for seniors with chronic conditions or disabilities.
The difference between nursing homes and assisted living facilities is the level of care. Assisted Living Facilities provide basic assistance related to Daily activities. where nursing homes provide round-the-clock care to patients, usually with chronic conditions.
Adult Day Care Centers
Adult daycare centers provide daytime care and supervision for seniors, allowing family caregivers to work or take respite. The National Adult Day Services Association estimates that more than 7,500 adult day service centers operate in the United States, serving over 260,000 participants and family caregivers.
Continuing Care Retirement Communities
Continuing Care Retirement Communities (CCRCs) offer a tiered approach to senior living, allowing residents to transition between levels of care as their needs change. There are more than 2000 CCRCs in the United States.
Other specialized care models include:
- Memory care facilities for seniors with Alzheimer’s disease or other forms of dementia,
- Hospice care for end-of-life support and
- Respite care services that provide temporary relief for primary caregivers.

Challenges in Caregiving
While the US caregiving industry has evolved to meet the growing needs of an aging population, it faces significant challenges, particularly regarding staffing availability and maintaining high-quality care. The COVID-19 pandemic further exacerbated these issues, putting an unprecedented strain on the healthcare system and highlighting existing vulnerabilities.
Staffing Availability
Staffing shortages represent one of the most pressing issues in the caregiving industry. According to the Bureau of Labor Statistics, the healthcare sector will experience 1.8 million new job openings between 2022 and 2032. Home health and personal care demand is forecast to grow faster than expected. In 2022, there were 3.7 million jobs for home and personal care aides, and over 800,000 workers were required by 2032. However, filling these roles has proven challenging. The 2021 American Health Care Association and National Center for Assisted Living (AHCA/NCAL) survey found that 99% of nursing homes and 96% of assisted living communities faced staffing shortages. These shortages continue into 2024
Several factors contribute to these staffing challenges:
- Low wages: Despite the demanding nature of caregiving work, compensation often remains low. In May 2023, the median annual wage for home health and personal care aides was $33,530, significantly below the median for all occupations.
- High turnover: The physically and emotionally demanding nature of caregiving work, combined with low pay and limited benefits, leads to high turnover rates. High turnover rates exceeding 85% are common across senior living facilities.
- Aging workforce: The caregiving workforce is aging, with over 55% of registered nurses over 50.
- Limited career advancement: Many caregiving roles offer limited opportunities for career growth, making it challenging to attract and retain talented individuals.
Quality of Care
These staffing challenges directly impact the quality of care provided to seniors. A study published in the Journal of the American Geriatrics Society found that higher nurse staffing levels in nursing homes were associated with better quality of care outcomes, including fewer pressure ulcers, less use of restraints, and fewer deficiency citations.
Quality of care is also affected by other factors:
- Training and education: The complexity of care required by many seniors, especially those with multiple chronic conditions or cognitive impairments, necessitates ongoing training and education for caregivers. However, training programs and standards vary widely across states and care settings.
- Regulation and oversight: While nursing homes are federally regulated, other care settings like assisted living facilities are primarily regulated at the state level, leading to inconsistent standards and oversight.
- Cultural competence: As the US senior population becomes more diverse, there’s a growing need for culturally competent care. However, the caregiving workforce only sometimes reflects the diversity of the population it serves.
- Technology adoption: While technology has the potential to improve care quality, its adoption in many care settings remains limited due to factors such as cost, training requirements, and resistance to change.
The COVID-19 pandemic, particularly pandemic-induced stress, further highlighted and exacerbated these challenges. As such, long-standing issues in nursing homes persist. These include staffing shortages, inadequate infection control, and underinvestment in quality improvement.
The Rise in Elder Abuse
A growing concern in the field of senior care is the rise of elder abuse, a problem that staffing shortages and inadequate oversight in some care settings have exacerbated. The National Council on Aging reports that approximately 1 in 10 Americans aged 60+ have experienced some form of elder abuse, with some estimates ranging as high as 5 million elders abused each year.

Elder abuse can take various forms, including physical, emotional, and sexual abuse, as well as neglect and financial exploitation. The National Center on Elder Abuse indicates that neglect is the most common type of elder abuse, often resulting from understaffing or inadequate training in care facilities. Additionally, financial exploitation of older adults is a form of elder abuse, costing $28.3 billion in losses each year. According to the National Council on Aging, typical forms of elder abuse include:
- Physical abuse means inflicting physical pain or injury upon an older adult.
- Sexual abuse means touching, fondling, intercourse, or any other sexual activity with an older adult when the older adult is unable to understand, unwilling to consent, threatened, or physically forced.
- Emotional/psychological abuse means verbal assaults, threats of abuse, harassment, or intimidation.
- Confinement means restraining or isolating an older adult other than for medical reasons.
- Passive neglect occurs when a caregiver fails to provide an older adult with life’s necessities, including, but not limited to, food, clothing, shelter, or medical care.
- Willful deprivation means denying an older adult medication, medical care, shelter, food, a therapeutic device, or other physical assistance and exposing that person to the risk of physical, mental, or emotional harm—except when the older, competent adult has expressed a desire to go without such care.
- Financial exploitation means the misuse or withholding of an older adult’s resources by another.
The COVID-19 pandemic has heightened these concerns. A study published in The American Journal of Geriatric Psychiatry found that reports of elder abuse increased by 83.6% during the pandemic, with social isolation and increased stress on caregivers cited as contributing factors.
Addressing the Challenges in Elder Abuse
Addressing this issue requires a multi-faceted approach:
- Improved screening and reporting mechanisms in healthcare settings
- Enhanced training for caregivers to recognize and prevent abuse
- Increased funding for adult protective services
- Stronger legal protections for elders
- Public awareness campaigns to educate about elder abuse
As the population ages and the demand for caregiving services grows, preventing elder abuse must be a priority to ensure the safety and well-being of vulnerable seniors.
Addressing the Challenges in Caregiving
Addressing these challenges will require a multi-faceted approach. Potential solutions under consideration include:
- Increasing wages and benefits for caregivers
- Developing career ladders and providing opportunities for advancement
- Improving working conditions and organizational culture in care settings
- Enhancing training programs and establishing more consistent standards across care settings. For example, use of LMS solutions for training can help streamline knowledge transfer processes.
- Leveraging technology to support caregivers and improve care efficiency.
- Implementing policies to attract more workers to the field, such as loan forgiveness programs for healthcare workers
- Improving data collection and quality measurement to drive improvements in care
As the demand for caregiving services continues to grow, addressing these staffing and quality-of-care challenges will be crucial to ensuring that seniors receive the high-quality care they need and deserve. The future of caregiving in the US will depend largely on building a robust, well-trained, and adequately compensated workforce supported by effective policies, technologies, and care models.
Ranking the Top 5 Caregiving Models in the US
To rank the most popular caregiving models in the US market, we’re considering several criteria: prevalence, flexibility, cost-effectiveness, quality of life, and family involvement. Based on these factors, here’s a ranking of the top 5 most popular caregiving models:
In-Home Care
This model tops the list due to its flexibility, cost-effectiveness, and ability to maintain seniors’ independence. Nearly 90% of seniors want to stay in their homes as they age. In-home care allows highly customizable care plans and promotes independence in familiar surroundings.
Assisted Living Facilities
These facilities balance independence and support well. The National Center for Assisted Living reports that 36% of residents stay in assisted living for one to three years, while 13% stay for more than five years.
Nursing Homes
While often viewed as a last resort, nursing homes are crucial in caring for seniors with complex medical needs. The CDC reports that about 1.3 million people receive care in skilled nursing facilities in the US. More than 85% are over age 65 or older, with 40% being over age 85.

Adult Day Care Centers
These centers provide valuable services for seniors needing daytime supervision and families balancing caregiving with work responsibilities. According to the National Adult Day Services Association, the average daily attendance at adult day centers is 25-30 participants. Presently, this model serves more than 800,000 nationwide.
Continuing Care Retirement Communities (CCRCs)
CCRCs offer a unique model that allows seniors to age in place while transitioning through different levels of care. While less widely available than other options, they are gaining popularity, particularly among more affluent seniors.
Emerging Trends in Caregiving in the US
The US caregiving industry is constantly evolving to meet the changing needs of seniors and their families. One significant trend is the integration of technology in caregiving. According to Grand View Research, the global digital health market was valued at $145.57 billion in 2021 and is expected to grow at a compound annual growth rate (CAGR) of 16.9% from 2022 to 2030. Technology in caregiving includes:
- Remote monitoring devices: The market forecasts expect a CAGR of 9.8% between 2023 and 2032, reaching USD 7.5 billion.
- Telehealth services: The market, valued at USD 120 billion in 2023, is expected to grow at a CAGR of 23.2% between 2023 and 2028. In the elderly segment, adoption rates continue to increase as accessibility and efficiency grow.
- Smart home technology: Given the high rates of seniors who prefer to age in place, these technologies are expected to address a range of pain points, such as safety and mobility for older consumers. Popular technologies include security systems, smoke detection, emergency contact systems, smart screens, etc.
- Virtual and augmented reality: These technologies can be used for cognitive stimulation and pain management. Devices such as Apple’s Vision Pro and Meta’s Quest 3 can potentially improve cognitive and mental health for residents and caregivers.
Another emerging trend is the focus on person-centered care, which emphasizes personalized, holistic care that considers physical needs and emotional, social, and spiritual well-being. This approach aligns with the growing demand for autonomy and choice among seniors.

Community and Informal Caregiving Models
The desire to age in place has led to innovations in home-based care models. According to the Village-to-Village Network, the village model expands the aging-in-place model to the aging-in-community. With roots in Boston in 2002, the number of villages has grown to over-grown, with 264 open villages and 55 in development across 43 states and 5 countries. These community-based membership organizations provide services to help seniors age in their homes, many of which are aligned with the WHO age-friendly cities.
Intergenerational care programs are also gaining popularity. According to Generations United, over 100 shared-site programs in the US now bring together seniors and younger generations.
As the prevalence of Alzheimer’s and other forms of dementia increases, there’s a growing focus on specialized memory care. The Alzheimer’s Association reports that 6.7 million Americans aged 65 and older are living with Alzheimer’s dementia in 2023, a number projected to rise to 13.8 million by 2060.
The caregiving industry also sees increased involvement from large corporations and franchise models. The home care franchise industry has experienced significant growth, with some of the largest franchises reporting annual revenue increases of 15-20%. In 2023, 16 of the top 400 franchises were in the home healthcare industry. Companies like Visiting Angels, Home Instead, and Griswold lead the list.
Informal and Unpaid Caregivers
There’s an increasing emphasis on caregiver support and training, recognizing the crucial role of both professional and family caregivers. The AARP estimates that about 38 million Americans provide unpaid care to adults with chronic, disabling, or serious health conditions. Moreover, the cost of this unpaid care totaled $600 billion. This highlights the need for support services for these informal caregivers. Key challenges for unpaid caregivers include:
- Emotional, physical, and financial strain
- Impact of the COVID-19 pandemic that exacerbated the challenges faced by unpaid caregivers
- Lack of workplace flexibility and support significantly impacts working caregivers.
- The unique challenges of racially, ethnically, and LGBTQ caregivers and LGBTQ

The Future of Caregiving in the US
In conclusion, senior caregiving in the United States is diverse and rapidly evolving, encompassing many models from traditional nursing homes to innovative tech-enabled home care and community solutions. As the population ages and preferences change, we expect continued innovation in this sector. In-home care remains the most popular model, aligning with seniors’ desire to age-in-place.
However, critical staffing shortages, issues with quality of care, and the rising concern of elder abuse must be adequately addressed. The COVID-19 pandemic has further exacerbated these challenges, highlighting the need for systemic changes in how we approach senior care. The pandemic’s effect on industry staffing will be felt for years. Moreover, as new elder care models, e.g., Villages and Intergenerational Care, emerge, workers must adapt to keep pace with the changing nature of care.
Looking ahead, the most successful caregiving models and caregivers will likely be those that can adapt to changing demographics, leverage new technologies, and provide personalized, holistic care that respects seniors’ dignity and autonomy. Simultaneously, addressing workforce issues, improving oversight and regulation, and implementing stronger protections against elder abuse will be crucial in ensuring high-quality care for all seniors. These challenges also offer new opportunities for entrepreneurs to create value from these emerging trends.
As we move forward, it will be essential to balance innovation with compassion, efficiency with quality, and independence with support. The future of caregiving in the US depends on our ability to meet these challenges head-on, creating a system that cares for our seniors and allows them to thrive in their golden years.
Disclosure: At ClearSky 2100, our portfolio partly consists of affiliate partnerships. We may earn a small commission from buying links on our site at no cost to you.





